The immune – metabolic link
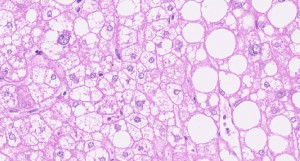
Haematoxylin/eosin (H/E) staining of a liver section derived from a human patient with NASH. Immune cell infiltrates, ballooning hepatocytes and fatty droplets are visible (courtesy of Professor Achim Weber).
Alterations in our way of living over the last decades, including high caloric intake (e.g. through high fructose and high fat diet) combined with a sedentary lifestyle, have augmented the incidence of overweight and metabolic syndrome, characterised by abdominal obesity, insulin resistance, hypertonia and dyslipidemia. This trend is observed not only in industrialised countries of the US or Europe but also step by step in developed as well as developing countries.
Overweight and metabolic syndrome lead to diseases of several kinds, including coronary heart diseases, Type 2 diabetes, and also cancer (e.g. liver, colorectal). Epidemiological data clearly indicate that overweight and metabolic syndrome are reaching pandemic dimensions in industrialised countries. Notably, it is suggested that newly developing countries – as a consequence of industrialisation and adaptation of their lifestyle – will also experience a steep increase in overweight and metabolic syndrome-triggered diseases. In the past ten years, the rate of obesity has doubled in adults and tripled in children in the USA A similar trend has also been observed in Europe.
The liver – which is the most important metabolic organ – is strongly affected by a chronic state of overweight and metabolic syndrome. Nonalcoholic fatty liver disease (NAFLD), the most frequent liver disease worldwide, is a clinical manifestation of overweight and metabolic syndrome. NAFLD is a chronic disease that can last several decades, characterised by predominant macrovesicular steatosis of the liver. Although the prevalence of NAFLD is increasing globally, epidemiology and demographic characteristics of NAFLD vary worldwide. It is becoming increasingly clear that a number of pathways are involved in the pathogenesis of NAFLD and NASH (nonalcoholic steatohepatitis) and its progression to advanced stages of liver disease. These pathways may be diverse in different cohorts of patients suffering from the condition, and understanding which pathways play a role in its development will be critical before launching treatment modalities.
A significant number of NAFLD patients develop nonalcoholic steatohepatitis (NASH), fibrosis and consequently hepatocellular carcinoma (HCC). In recent years, obesity, leading to metabolic syndrome, steatosis and steatohepatitis, has attracted increased attention due to an increased HCC incidence in the US and Europe. In line with this, the most common etiology for HCC in industrialised countries has recently switched from chronic viral infections (e.g. hepatitis B and hepatitis C virus) to obesity, making HCC the most rapidly increasing type of cancer in the US, with a similar trend observed in Europe. Today we lack a detailed understanding of how chronic steatosis develops into NASH and what factors control its transition from NASH to HCC. At the same time, no therapeutics exist to efficiently treat NASH, and treatment options for the therapy of late stage HCC are limited and prolong the lifespan of patients for between three to six months.
In laboratory mice, NASH can be induced by several different diets, such as a methionine/choline-deficient (MCD) or choline-deficient diet (CD) but not by a high-fat diet (HFD) alone. However, C57BL/6 mice fed with MCD or CD do not develop obesity or metabolic syndrome, and the diet has to be discontinued after a few months due to weight loss (up to 40%) or occasional cachexia. Hence, these approaches do not recapitulate NASH and its consequences (e.g. transition to HCC) in humans, and appropriate mouse models for genetically and mechanistically dissecting NAFLD-induced NASH and NASH-triggered HCC development have been thus far lacking.
Deficiency in the essential nutrient choline was described in NAFLD patients to exacerbate NAFLD and NASH. Moreover, humans with inadequate choline uptake were shown to have defects in hepatic lipoprotein secretion, oxidative damage caused by mitochondrial dysfunction and ER stress.
Based on the clinical observations of choline deficiency to exacerbate NAFDL and NASH patients, we have recently combined choline deficiency with a high fat diet (CD-HFD) as a chronic diet for laboratory mice, which may lead to metabolic syndrome, steatosis, liver damage and NASH, thus delivering the ‘second hit’ that promotes dietary-induced liver carcinogenesis – similar to the human situation. This approach has enabled us to establish a chronic mouse model of NASH and metabolic syndrome, triggering subsequent HCC in a wild-type C57BL/6 mouse, in the absence of chemical carcinogens or genetic mutations predisposing to NASH or HCC development (Wolf **it et al., Cancer Cell, 2014). CD-HFD-treated mice display obesity, overweight, insulin resistance, liver damage and fibrosis and hepatic mitochondrial damage, dyslipidemia and NASH, as observed in human patients. HCC developed 12 months post-CD-HFD start and resembled histologically, genetically and morphologically human HCC. Interestingly, by using this novel model we could show that adaptive immune cells (e.g. cytotoxic T-cells as well as natural killer T cells) greatly contribute to the diet-induced liver pathology. Consequently, we also analysed NASH patients and patients suffering from other liver diseases with concomitant lipid deposition diseases (e.g. chronic HCV infection) and could find the same activated immune cells in livers of NASH patients, as well as the same cytokines, which we identified to be causally linked to NASH and HCC disease development.
We thus believe that our mouse model recapitulates several pathophysiological aspects of human NASH and enables us to study its development and transition to HCC. In the future, the link between activated T-cells in the liver and their crosstalk to hepatocytes could give us important insights into how we can generate novel therapeutics for treating NASH as well as NASH-induced HCC in industrialised countries.
References:
Wolf M J, Adili A, Piotrowitz K, Abdullah Z, Boege Y, Stemmer K, Ringelhan M, Simonavicius N, Egger M, Wohlleber D, Lorentzen A, Einer C, Schulz S, Clavel T, Protzer U, Thiele C, Zischka H, Moch H, Tschöp M, Tumanov A V, Haller D, Unger K, Karin M, Kopf M, Knolle P, Weber A, and Heikenwalder M. Metabolic activation of intrahepatic CD8+ T-cells and NKT cells causes non-alcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. **it Cancer Cell. 13 October 2014;26(4):549-64. doi: 10.1016/j.ccell.2014.09.003
Mathias Heikenwälder
Institute of Virology
Helmholtz Zentrum München (Helmholtz-Zentrum für Gesundheit und Umwelt (HMGU)/ Technische Universität München (TUM)
Schneckenburgerstrasse 8
81675 München
tel: +49-89-4140-7440
[email protected]
www.virologie.med.tu-muenchen.de/en/forschung-tum/ag-heikenwalder/
